60 Second Summary
Atopic dermatitis (AD), also known as eczema, is the most common skin condition in children (30% prevalence in the first 2 years) and second most common in adolescents and adults (7% prevalence) after acne. The cause of AD relates to a combination of the triad of skin barrier dysfunction, skin dysbiosis, and dysfunctional inflammation. AD is associated with other atopic conditions such as food allergy, asthma, and allergic rhinitis. These associations often lead to patients with AD being treated with ineffective and inappropriate treatments, such as dietary restriction, which have no role in AD.
To deal with the three intertwining causes of AD, a three-pronged approach is necessary: emollients to replenish the skin barrier, topical steroids or calcineurin inhibitors to reduce inflammation, and antiseptic bleach baths to reduce cutaneous dysbiosis. In special scenarios oral antibacterial or antiviral agents may be required.
Patients with AD should NOT be told to use topical steroids ‘sparingly’ or ‘thinly’ and should be advised to treat for an adequate duration. Patients with AD should NOT be treated with oral steroids (outside of expert centres with a therapeutic exit strategy in place) due to the severe side effects and lack of disease modification. Patients with AD should NOT be told to change their washing powder or reduce/eliminate foods from their diet, as AD is not caused by detergents or food allergy.
Patients with persistent or severe AD despite the use of appropriate potent topical therapy should be referred to dermatology for consideration of advanced therapies.
Introduction
Atopic dermatitis (AD), also known as eczema, is the most common skin condition in children (up to 30% prevalence in the first 2 years of life and 20% overall) and second most common in adolescents and adults (7% prevalence) after acne. AD has a significant impact on quality of life (QOL), and children with severe AD have worse QOL than children with type 1 diabetes mellitus or treatment-resistant epilepsy. The main burdensome symptoms are itch and sleep disruption (Images 1A-1D). AD is associated with other atopic conditions such as food allergy, asthma, and allergic rhinitis. These associations often lead to patients with AD being treated with ineffective and inappropriate treatments, such as dietary restriction, which have no role in AD. AD is also associated with neuropsychiatric disease such as anxiety, depression, and attention- deficit hyperactivity disorder.

Cause of AD
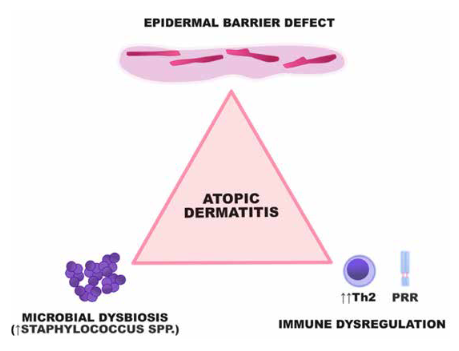
The cause of AD relates to a combination of the triad of skin an important role in the skin’s barrier function. It brings together
structural proteins in the outermost skin cells to form tight bundles, flattening and strengthening the cells to create a strong barrier. In AD, skin is heavily colonised with Staphylococcus aureus (S. aureus) in lesional and non-lesional skin. A rising proportion of S. aureus in skin microbiome samples predicts a flare, and diversity of non-staphylococcal species returns once a flare has been treated. A hallmark of AD is Th2-mediated inflammation, with high levels of IL-4 and IL-13 that promote dysfunctional allergic inflammation. With chronic or untreated AD, other immune pathways can become activated. Each component of the triad interacts with the others in a vicious cycle, for example filaggrin deficiency allows antigens to penetrate the stratum corneum and stimulate inflammation, and subsequently IL-4 and IL-13 production leads to reduced filaggrin production. It has recently been shown that dupilumab (a biologic targeting IL-4 and IL-13) not only reduces inflammation but enhances skin barrier function, highlighting the importance of adequately treating inflammation in AD. It is essential to treat each component of the causes of AD adequately to optimise outcomes.
Treatment of AD
Anti-inflammation
The use of anti-inflammatory steroid creams/ointments is essential to reduce inflammation in AD. Early and aggressive use of topical steroids can reduce the duration of disease, and may also reduce the risk of developing associated problems. The dermatology team in Crumlin have recently shown that reducing inflammation in the skin using steroid creams also reduces systemic inflammation, suggesting that topical steroids can correct the systemic immune dysregulation in AD. For mild AD, hydrocortisone 1% can be dispensed over the counter. However, hydrocortisone 1% is a very weak anti-inflammatory agent, and is not sufficient to treat more severe eczema. For moderate AD, agents such as clobetasone butyrate (Eumovate) or betamethasone valerate 0.025% (Betnovate RD) can be used. For severe AD, potent agents such as betamethasone valerate 0.1% (Betnovate 0.1%) or mometasone furoate (Elocon) should be used (Image 3). In general it is better to use a more potent topical steroid less frequently than a weaker topical steroid more frequently, for two reasons: systemic absorption is related to the frequency of application, and the burden of treatment with daily topical steroid application is much higher than twice weekly. Topical steroids should be applied liberally (not sparingly!) so that the affected skin is left glistening afterwards. Ointments are preferable to creams as the higher lipid content makes the vehicle more effective. There is no benefit to using topical steroids more than once daily – more frequent use increases the risk of systemic absorption and reduces patient adherence. In general, therapy should be continued once daily for two weeks, then weaned to alternate days for two weeks, then maintained twice weekly (weekend therapy on Saturdays and Sundays is a good option for busy parents/patients) until the skin has been clear for several months.
Myth 1 Topical steroids should be applied sparingly/thinly and only for short bursts
Topical steroids are a very elegant way to deliver local anti-inflammatory therapy, without the potential side effects that systemic therapy can produce. Skin that is inflamed with AD is on fire immunologically. This immune dysregulation needs to be extinguished appropriately to prevent worsening or chronic AD. If topical steroids are stopped too quickly the inflammation can return rapidly. Parents are almost always counselled by pharmacists and non-dermatology doctors about the risk of skin thinning, but this is generally limited to prolonged use of extremely potent topical steroids such as Dermovate (which should only be prescribed for palmoplantar AD). We have recently performed qualitative research interviewing parents of children with severe eczema, and the ‘mixed messages’ about the safety of topical steroids can cause significant upset.
Myth 2 Topical steroids can never be used on broken skin in AD
When skin inflammation is so severe that it has caused skin breakdown, either directly or indirectly from scratching, it is essential to reduce inflammation to avoid further damage. It is safe to apply topical steroids to broken skin.
Topical tacrolimus, a calcineurin inhibitor, is an alternative to topical steroids. It is a useful anti-inflammatory adjunct, particularly in the maintenance phase of AD (rather than the treatment of flares, when it is less effective than potent topical steroids). The only side effect is mild stinging with the first few applications, which usually settles down with ongoing use. Given the lack of steroid, it is particularly useful for sensitive areas such as the eyelids. Topical tacrolimus is much more expensive than topical steroids.
Myth 3 Topical tacrolimus can never be used in babies and only 0.03% can be used in older children
Topical tacrolimus (Protopic) has been used in dermatology for decades, with an overwhelming volume of reassuring safety data. Protopic 0.1% is licensed for patients over 16 years, and Protopic 0.03% is licensed from two to 16 years. Dermatologists usually prescribe the 0.1% formulation for all ages, because of the extensive safety data and the enhanced efficacy. There is extensive anecdotal evidence of safety of Protopic in younger infants, so Protopic 0.1% is often prescribed off-license for infants under two years.
Skin barrier replenishment
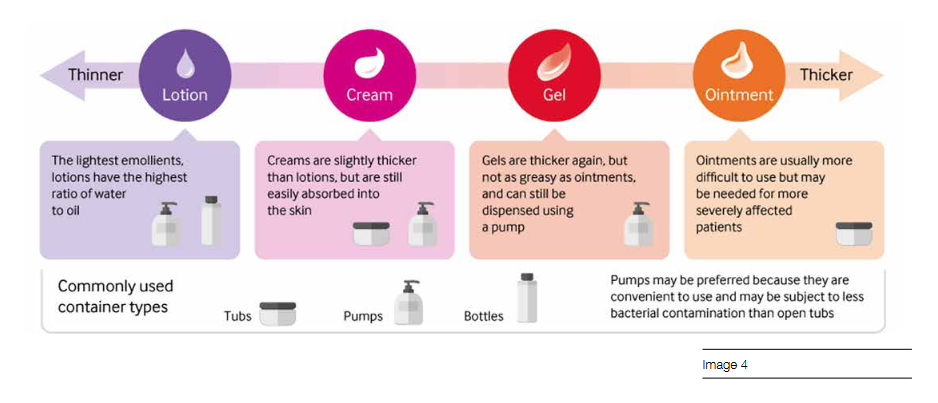
Moisturisers (also known as emollients) should be used twice daily or more, and moisturising after a bath (‘soak and seal’) is an excellent way to hydrate the skin. Moisturisers should be applied downwards to avoid blocking or irritating hair follicles. A pump dispenser is useful for preventing bacterial colonisation of the oisturiser container. Alternatively, a large spoon can be sterilised (using boiling water) and dipped into a tub to avoid transfer of bugs from the parent’s hand to the container (Image 4). Appropriate bathing/showering advice for AD is to avoid soaps or irritant products that produce bubbles, use an emollient (that does not contain sodium laureth sulfate) as a wash, keep the temperature of the bath/shower tepid, and limit the duration of the bath/shower to 10 minutes or less. The skin should be gently patted dry afterwards.
Myth 4 There is a number one brand of emollient for treating AD
There is no particular brand of emollient that is significantly superior than any other for treating AD. One of the key causes of AD is an impaired skin barrier, and every individual has differing levels of various proteins in their skin that retain moisture and protect us from external threats. Every moisturiser has a different mixture of ingredients, so it is best for patients/parents to try several brands to see which leaves the skin most hydrated.
Antimicrobial strategies
For infection-driven flares, the addition of sodium hypochlorite (Milton) is an effective strategy for reducing microbial colonisation, without causing antibiotic resistance. Two capfuls (60mL) can be added to a baby bath (50L) and four capfuls (120mL) can be added to a full bath (100L).
Topical fusidic acid (Fucidin) should be prescribed with caution and other skin infections. S. aureus resistance to fusidic acid has reached crisis point, driven by inappropriate use of topical antibiotics. Moreover, the selection for fusidic acid resistant strains also selects for methicillin resistance, creating even more problems with MRSA. If antibiotics are required for infected AD, then oral antibiotics should usually be prescribed, in conjunction with topical antiseptics (eg Milton).
Myth 5 Topical antibiotics are better than oral antibiotics because they do not cause antimicrobial resistance
Topical antibiotics are known to cause localised antimicrobial resistance in the area being treated, but also in cutaneous sites distant to application. One recent study even showed antimicrobial resistance on the skin of close contacts. While oral antibiotics have scope to cause more antimicrobial resistance in an individual patient due to exposure to other flora such as in the gastrointestinal tract, topical antibiotics are usually washed off ‘as is’, compared to oral antibiotics which are excreted in urine or egested in faeces as less active or inactive by-products. The introduction of topical antibiotics directly to waste water is a major contributor to antimicrobial resistance globally.
Special scenarios Bacterial superinfection
As mentioned, S. Aureus is a significant factor in the pathogenesis and flares of AD. While patients with AD are almost always colonised with S. aureus, some patients will develop bacterial superinfection. This manifests as weeping of clear or purulent fluid, honey-coloured crust, folliculitis, abscess, or cellulitis (Image 5). If there is evidence of bacterial superinfection then oral antibiotics should be prescribed, guided by microbiological cultures (predominantly for resistance information) and local antimicrobial practices. These should be prescribed in conjunction with topical antiseptic measures, which should be instituted as a preventative measure.

Eczema herpeticum
Eczema herpeticum occurs due to infection with herpes simplex virus, and is more common in children. It manifests as clusters of painful and itchy blisters which evolve into punched-out erosions, sometimes associated with fever (Image 6). Patients can have inactive AD, so it does not represent a sign of treatment failure. It is helpful to take viral PCR swabs to confirm the diagnosis. Treatment should be immediately started with aciclovir. Oral acyclovir/valaciclovir is acceptable unless there is concern for ophthalmic or central nervous involvement, or if the patient is unwell. Patients with recurrent eczema herpeticum should consider prophylactic antiviral treatment.
Eczema coxsackium
Eczema coxsackium is a recently described entity caused by coxsackie A6 or A16 in patients with AD. Clusters usually occur in springtime. It looks very similar to eczema herpeticum but it is not itchy and there is a slightly purpuric hue to the background skin (Image 7). Respiratory viral panels can be sent to confirm enterovirus infection as the PCR testing is difficult to access. Given the similarities to eczema herpeticum it is very reasonable to start treatment with acyclovir or valaciclovir but enteroviruses do not express viral thymidine kinase and therefore do not respond to antiviral treatment.
What NOT to do
Patients with AD should NOT be told to use topical steroids ‘sparingly’ or ‘thinly’ and should be advised to treat for an adequate duration. The consequences of undertreated AD are huge, and the terrible impact on QOL is unnecessary given the safety and efficacy of topical steroids. Patients with AD should NOT be treated with oral steroids (outside of expert centres with a therapeutic exit strategy in place) due to the severe side effects and lack of disease modification. Patients will improve rapidly within a few days of high dose oral steroids but will flare even worse once withdrawn. Given that we now have effective targeted treatments for AD in specialist clinics there is no excuse for inappropriate prescriptions of oral steroids. Patients with AD should NOT be told to change their washing powder or reduce/eliminate foods from their diet. AD is absolutely not caused by detergent! In children who have co-morbid AD and food allergy, if an allergenic food is removed from the diet it will not affect the AD but will simply stop immediate IgE-mediated allergic reactions from happening.
When to refer
Patients with persistent or severe AD despite the use of appropriate potent topical therapy should be referred to dermatology for consideration of advanced therapies. Use of 1% hydrocortisone for a few days does not represent a trial of topical steroids: an adequately potent steroid should be prescribed for at least two weeks to assess response. Dermatologists now have access to dupilumab, a biologic drug targeting IL-4 and IL-13 which can be life-changing for patients who have lived with severe itch for years or even decades. In addition, other biologic drugs such as tralokinumab (IL-13 inhibitor) and oral janus kinase (JAK) inhibitors such as upadacitinib or abrocitinib are also available. JAK inhibitors have a more rapid onset of action and quickly reduce itch, but there are still some concerns about long-term use, based on studies in other conditions such as rheumatoid arthritis, with patients who represent a very different population to those with AD. Topical JAK inhibitors have been licensed in some countries with significant benefit seen in AD, although cost is currently prohibitive.
Overall it is a very positive time for dermatologists and patients with AD, with effective treatments already available and many more in the pipeline.