60 Second Summary
The number of HIV diagnoses in Ireland is alarming with approximately 8 people diagnosed with HIV every week. This is despite the introduction of several initiatives to tackle the spread of the disease.
Human Immunodeficiency virus (HIV) is a disease of major public health significance in Ireland and across the world. It is the causative agent of acquired immune deficiency syndrome (AIDS) which causes millions of deaths every year.
HIV is found in all bodily fluids but is only present in infectious quantities in genital fluids (vaginal fluids, semen and moisture in the rectum), blood and breast milk. HIV is not infectious in saliva, urine, faeces or tears.
When a person is infected with HIV, the virus replicates in the CD4 T cells within a few days. This stage of HIV infection is referred to as sero-conversion and is characterised by a strong immune response as the body tries to fight the infection. In the days to weeks following initial HIV exposure, individuals experience flu like symptoms such as headaches, fever, sore throat and a rash. At this stage, the viral load is extremely high, and there is a high risk of disease transmission.
Stigma around HIV stems back to its original discovery in gay men in the 1980s where HIV was incorrectly referred to as ‘gay cancer’ or the ‘gay plague’. These misconceptions around the disease are still present today and have an enormous impact on those living with HIV.
The ultimate goal of HIV treatment is to achieve viral suppression, where HIV is undetectable in the blood. Treatment of HIV includes ART, the management of opportunistic infections or malignancies, the management of ‘non-HIV related’ co-morbidities and symptom control.
AUTHOR: Written by Caoimhe Jameson, Community Pharmacist Caoimhe Jameson is a pharmacist currently working with TCP Homecare. She graduated from Trinity College in 2020 and has experience in community pharmacy and the addiction services, where she worked as the Hepatitis C Pharmacist in the National Drug Treatment Centre. Since graduating as a pharmacist, Caoimhe has completed a diploma in Leadership and Change Management from the University of Sunderland.
1. REFLECT – Before reading this module, consider the following: Will this clinical area be relevant to my practice?
2. IDENTIFY – If the answer is no, I may still be interested in the area but the article may not contribute towards my continuing professional development (CPD). If the answer is yes, I should identify any knowledge gaps in the clinical area.
3. PLAN – If I have identified a knowledge gap – will this article satisfy those needs – or will more reading be required?
4. EVALUATE – Did this article meet my learning needs – and how has my practise changed as a result? Have I identified further learning needs?
5. WHAT NEXT – At this time you may like to record your learning for future use or assessment. Follow the 4 previous steps, log and record your findings.
Published by IPN. Copies can be downloaded from www.irishpharmacytraining.ie
Disclaimer: All material published is copyright, no part of this can be used in any other publication without permission of the publishers and author.
The number of HIV diagnoses in Ireland is alarming with approximately 8 people diagnosed with HIV every week.1 This is despite the introduction of several initiatives to tackle the spread of the disease. There is also an overwhelming amount of disinformation around HIV. With over 2 million visits to the community pharmacy each month in Ireland, community pharmacists are well placed to dispel myths around HIV and play a pivotal role in both the prevention of HIV transmission as well as the provision of care for those living with HIV. 2 This can be achieved by community pharmacists normalising conversations about HIV and sexually transmitted diseases and providing information on how to get tested. If an individual is diagnosed with HIV their treatment is provided through hospital-based services, however community pharmacists can continue to provide advice particularly on potential drug interactions and harm reduction methods.
This article aims to support community pharmacists by providing an overview of the HIV virus including its transmission, testing methods and treatment.
Human Immunodeficiency virus (HIV)
Human Immunodeficiency virus (HIV) is a disease of major public health significance in Ireland and across the world. It is the causative agent of acquired immune deficiency syndrome (AIDS) which causes millions of deaths every year. HIV disproportionately affects certain population groups, including people who inject drugs (PWIDs), men who have sex with men (MSM) and sex workers, due to the way in which it is transmitted. Over 6,000 people are estimated to be living with HIV in Ireland and it is thought that about 15% of these people do not know yet that they have HIV.3
HIV is a retrovirus which attacks the CD4 T lymphocytes (CD4 T cells) of the immune system. CD4 T cells coordinate the immune response by stimulating other immune cells to fight infection. The stages of disease progression from when an individual is infected with HIV to the development of AIDS is described in stages. In the 1980s, a diagnosis of HIV infection ultimately advanced to AIDS however due to the development of antiretroviral treatment (ART) this is no longer the case. Treatment with ART prevents disease progression such that a person on life-long ART has a life expectancy similar to that of the general population.4
The stages of HIV infection
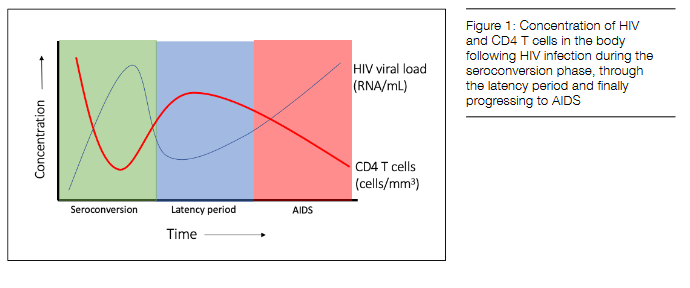
When a person is infected with HIV, the virus replicates in the CD4 T cells within a few days. This stage of HIV infection is referred to as sero-conversion and is characterised by a strong immune response as the body tries to fight the infection. In the days to weeks following initial HIV exposure, individuals experience flu like symptoms such as headaches, fever, sore throat and a rash. At this stage, the viral load is extremely high, and there is a high risk of disease transmission.
Following the sero-conversion stage, a latency period occurs where there are no signs or symptoms of the disease. This latency period may last for several years and without being tested, individuals may not be aware of their infection. During this period, as the HIV viral load increases, the number of CD4 T cells is slowly depleting. ART prevents an increase in the HIV viral load and prevents the disease progressing past the latency phase. Measuring the CD4 T cell count estimates the level of immunosuppression as a result of HIV. This measurement is the number of CD4 T cells in a sample of the individual’s blood. The normal range can vary between 500 and 1500 cells/mm3.
At a CD4 T cell count below 350 cells/mm3, individuals can become symptomatic as a result of opportunistic infections. Initially symptoms may be mild such as fatigue, weight loss, mouth ulcers and thrush but as the disease progresses the symptoms worsen. AIDS is typically diagnosed by a CD4 T cell count below 200 cells/mm3 accompanied with a high viral load and opportunistic infections and cancers known as AIDS-defining illnesses.
HIV Transmission
HIV is found in all bodily fluids but is only present in infectious quantities in genital fluids (vaginal fluids, semen and moisture in the rectum), blood and breast milk. HIV is not infectious in saliva, urine, faeces or tears.
This is a common misunderstanding in the general population. 70% of respondents to a study conducted by HIV Ireland in 2017, believed that HIV can be transmitted through a bite and 24% believed it can be transmitted by kissing.5 This highlights a need for continued public education around this topic as these inaccurate beliefs are harmful and can add to stigma around HIV.
HIV cannot be transmitted through coughing, sneezing, spitting, kissing, hugging, shaking hands, animal or human bites. Furthermore, if an individual with HIV is taking lifelong ART and they have an undetectable HIV viral load, they cannot pass on the virus. In the same 2017 report, only 19% of respondents correctly reported this.5 The global awareness campaign “Undetectable=Untransmittable” or “U=U” aims to eliminate HIV stigma and discrimination.6
The main ways HIV is transmitted is through unprotected anal, vaginal and oral sex. HIV transmission also occurs:
– through the sharing of unsterilised injecting equipment which is infected with HIV due to being previously used by someone who is HIV positive
– during pregnancy, childbirth or breastfeeding, from the HIV-positive parent who is not taking HIV treatment to their baby
– through receiving donated blood or organs infected with HIV, or injections with unsterilised needles carrying the virus in countries with inadequate screening and infection control procedures.
Not every act of unprotected sex with an HIV-positive person results in HIV transmission. In addition to the type of sex, other factors can affect the risk that an exposure to HIV leads to infection. These include the presence of STIs, a high viral load, a man being uncircumcised, a woman menstruating, other bleeding and activities that can cause tearing and inflammation.
In 2018 in Ireland, MSM accounted for 56% (n=293) of HIV diagnoses in Ireland; 3% of new diagnoses were among PWID and heterosexual transmission accounted for 31% of HIV diagnoses.7 Access to HIV testing and treatment is free for everyone in Ireland, however everyone may not know how to avail of these services. Having an understanding of health disparities and initiating conversations and interventions in the community pharmacy can help to address this shortcoming.
Stigma around HIV stems back to its original discovery in gay men in the 1980s where HIV was incorrectly referred to as ‘gay cancer’ or the ‘gay plague’. These misconceptions around the disease are still present today and have an enormous impact on those living with HIV. Negative attitudes towards HIV can lead to individuals feeling isolated and unsupported, which in turn can have a significant impact on their physical and mental health. Initiating conversations in the pharmacy and tackling misbeliefs through education has the potential to reduce this stigma.
Prevention of HIV Transmission
Effective strategies to prevent sexual acquisition of HIV include the use of HIV testing, condoms, health promotion and risk reduction education, pre-exposure prophylaxis (PrEP), post exposure prophylaxis following sexual exposure (PEPSE) and treatment as prevention (TasP). Signposting individuals to these services may empower them to engage with them.
Free condoms are available from sexual health clinics, sexual health organisations (e.g., HIV Ireland) and many third level colleges. www.sexualwellbeing. ie is an excellent resource to refer individuals to for support around their sexual health and wellbeing.
HIV is tested for as part of routine STI screening in Ireland. HSE public STI screening services are almost exclusively based in hospitals and community clinics around Ireland and are free of charge and confidential. A full list can be found on www.sexualwellbeing.ie. Private STI screening is also available such as through GPs and private clinics.
SH:24 is a free online sexual health service, delivered in partnership with the HSE in Ireland and the NHS in the UK. Sexually transmitted infection (STI) test kits can be ordered at www.sh24.ie and are posted to a person’s home along with instructions and a return envelope to send the completed kit back to the lab. Results are received by text message within 72 hours of the sample arriving at the lab. This service is anonymous and non-judgemental and anyone with a positive result will be contacted by the SH:24 team to organise free assessment and treatment.

When providing advice to individuals on HIV testing it is important to consider the ‘window period’. The window period is the term used to describe the time between someone getting infected with HIV and developing a positive HIV test which can be up to 12 weeks.8 Repeat testing after the ‘window period’ is often advised after an initial negative test. There are several types of HIV tests: antibody tests, antigen/antibody tests and nucleic acid tests. No HIV test can detect HIV immediately after exposure due to the window period, which varies depending on the test.
– Antibody tests: This tests for HIV antibodies which are produced after exposure but can take up to 12 weeks to develop. Antibody tests are usually a venous blood sample, a finger stick blood sample or an oral fluid sample.
– Antigen/antibody tests: The p24 HIV antigen is present in high levels in newly infected individuals so can be useful for early detection of HIV. Once p24 antibodies are produced, the p24 antigen may become undetectable so a combined antigen/antibody test is more useful for diagnosing HIV. The estimated window period is 18-45 days.
– Nucleic acid test (NAT): This test is for the virus itself in the blood, it is also known as a HIV viral load test. It can detect HIV sooner than other types of tests. The window period is estimated at 10-33 days.
PrEP
PrEP is the pre-emptive use of oral ART by HIV-negative individuals to reduce the risk of HIV infection. Generic PrEP became available in Ireland in December 2017 increasing its affordability.9 A full list of approved PrEP services can be found at www.sexualwellbeing. ie. PrEP is available for free in Ireland to HIV negative individuals who are aged 17 years or older, have a PPSN and fall into one of the following categories:
1: Men who have sex with men or transgender women who have sex with men who are: – Sexually active with likelihood of remaining sexually active in the next 3 months AND one of the following:
– reported condomless anal sex with at least two partners over the last 6 months
– episode of documented or reported acute STI over the last 12 months
– documented or reported use of HIV PEPSE over the last 12 months
– reported engagement in chemsex (the use of drugs as part of one’s sex life) over the last 6 months
2. Individuals having condomless sex with a HIV positive person who is not stably suppressed on antiretroviral therapy, specifically:
– where the person living with HIV is not on antiretroviral therapy
– where the person living with HIV has initiated antiretroviral therapy but has not yet achieved virological suppression.
– where the person living with HIV has loss of virological control on antiretroviral therapy and the risk of HIV transmission has been deemed by a consultant physician specialising in HIV Medicine to be substantial and warrant PrEP for the HIV-negative partner
3: Other heterosexual men, heterosexual women considered by a senior clinician specialising in HIV Medicine to be at substantial risk for sexual acquisition of HIV.
There are some situations where PrEP is not recommended including in individuals unwilling to attend for follow up, those with significant renal impairment at baseline and those who report sub-optimal adherence with continued significant risk for sexual acquisition of HIV due to the risk of antiretroviral resistance. PrEP prescriptions are usually for three months at a time and individuals must commit to regular follow up appointments.
Event based dosage of PrEP has been shown to be effective for men who have anal sex with other men and can be considered where sex is infrequent (less than 2 times per week) and where the individual is able to allow adequate time for taking the first dose before having sex. Event-based dosage is not recommended for women (including transgender women); transgender men having vaginal sex; men having vaginal sex or anal sex with women and people who are hepatitis B surface antigen positive.
PEP
PEP (post-exposure prophylaxis) is a short course of ART that can be taken to prevent HIV infection within 72 hours of exposure to the virus. The first dose of PEP should be given as soon as possible, ideally within 2 hours of exposure. PEP is available through STI clinics and emergency departments; the latter should be reserved for when it is not possible to get PEP from a local STI clinic within 72 hours. A full course of PEP is 28 days however emergency departments often only supply starter packs for three days and refer the person for further assessment for continued treatment.10 PEP is free in Ireland however, individuals who attend the emergency department without a referral letter, unless exempt, will be charged ¤100. Often the community pharmacy is the first port of call for health advice especially at the weekend. Providing information and signposting individuals to the appropriate services will enable individuals to obtain PEP in a timely manner. A full list of clinics and emergency departments providing PEP can be found at www.sexualwellbeing.ie.

Needle exchange
Pharmacy based needle exchange is a service that has the potential to dramatically impact the spread of HIV and other blood borne viruses (BBVs). In 2012, across 63 pharmacies offering needle exchange, 33 had transactions where they provided injection equipment packs along with information leaflets on safer injecting advice and harm reduction. 11
Antenatal testing
A national voluntary programme of HIV antenatal screening has been in place in Ireland since 1999. As part of this programme, it is recommended that HIV testing be offered to all women who attend for antenatal services. In 2019, Nine women were newly diagnosed with HIV at their antenatal screen.12
HIV Treatment
The ultimate goal of HIV treatment is to achieve viral suppression, where HIV is undetectable in the blood. Treatment of HIV includes ART, the management of opportunistic infections or malignancies, the management of ‘non-HIV related’ co-morbidities and symptom control.
In July 2017, the HSE adopted the position that all individuals living with HIV attending HIV services in Ireland are to be offered ART free of charge and informed of the benefits of ART in improving their personal health and reducing HIV infectiousness.
ART is one of the fastest evolving areas of medicine and has transformed a HIV diagnosis from inevitably progressing to AIDS to a manageable disease that one can live a relatively normal life with. ART is not a cure for HIV, it stops the virus from reproducing in the body and can reduce the viral load to undetectable levels. Once ART is started and the individual adheres to the treatment regime, the virus can become undetectable within 6 months. Adherence is incredibly important, and the community pharmacist can provide support to facilitate this.
Achieving viral suppression improves health outcomes for individuals living with HIV, allowing them to have an improved quality of life and live longer. Viral suppression prevents the spread of HIV as individuals who have an undetectable viral load have effectively no risk of transmitting HIV to their sexual partners.
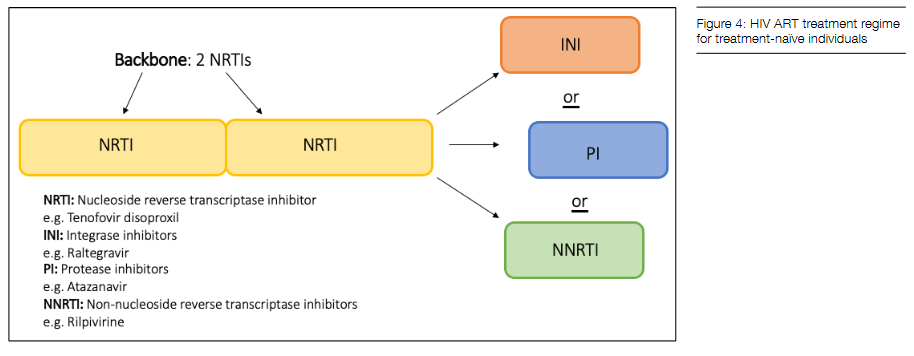
Commonly known as triple therapy, a combination of three antiretroviral agents, selected on the basis of treatment history and resistance tests, should usually be prescribed to increase efficacy and reduce the development of drug-resistant virus. Treatment-naïve individuals should start with a non-nucleoside reverse transcriptase inhibitors (NNRTIs) backbone in combination with a third agent regardless of their CD4 T cell count. Combination medications such as Truvada (emtricitabine and tenofovir disoproxil), Descovy (emtricitabine and tenofovir alafenamide fumarate) and Biktarvy (bictegravir sodium, emtricitabine and tenofovir alafenamide fumarate) can aid compliance.
In the community pharmacy it is important to be aware of drug interactions with ART for HIV. The University of Liverpool drug interaction checker (www.hiv-druginteractions.org) is a useful tool which can be used to check for drug interactions. Some ART drugs are substrates of certain CYP enzymes and so inducers and inhibitors of these enzymes can affect their concentrations. When counselling individuals on over the counter and prescription items, it is vital to check if they are on any other medication. For individuals taking triple therapy, drug interactions should be ruled out to ensure treatment efficacy is not affected.
Opportunistic infections occur in individuals with HIV when their immune system is compromised. Examples are pneumocystis carinii pneumonia (PCP) and tuberculosis (TB). Cotrimoxazole is a commonly used antibiotic to prevent opportunistic infections in individuals with HIV.
In Ireland, HIV care is provided in nine hospitals. Adult care is provided in Cork (Cork University Hospital), Dublin (Beaumont Hospital, Mater Misericordiae University Hospital, St. James’s Hospital, St. Vincent’s University Hospital), Galway (Galway University Hospital) and Limerick (Limerick University Hospital). Paediatric HIV care is provided in Dublin at Temple St. University Hospital and Our Lady’s Children’s Hospital.
The role of the community pharmacist is ever evolving and there is potential for involvement in services such as HIV testing, like our counterparts in the USA and Canada. 13 Using a holistic approach to support individuals living with HIV, the community pharmacist can have a positive impact on their life and treatment outcomes.
References available on request
5 questions and answers for the readers to ensure they understand the article:
1. Q: What are the main stages following infection with HIV.
A: (1) Sero-conversion (2) Latency period (3) AIDS
2. Q: What is a CD4 T cell count?
A: This measurement is the number of CD4 T cells in a sample of an individual’s blood. The normal range can vary between 500 and 1500 cells/mm3.
3. Q: What is the main way in which HIV is transmitted?
A: The main ways HIV is transmitted is through unprotected anal, vaginal and oral sex.
4. Q: Where can an individual access PEP?
A: PEP is available through STI clinics and emergency departments; the latter should be reserved for when it is not possible to get PEP from a local STI clinic within 72 hours.
5. Q: What are the constituents of a HIV ART treatment regime for treatment-naïve individuals?
A: Treatment-naïve individuals should start with a non-nucleoside reverse transcriptase inhibitors (NNRTIs) backbone in combination with a third agent regardless of their CD4 T cell count.










