60 Second Summary
The common cold and flu are both viral upper respiratory tract infections. Symptoms are generally self-limiting, with symptoms of a cold including blocked or runny nose, sneezing, cough and sore throat.
Symptoms of flu include fever, fatigue, body aches, headache, dry cough and nausea. Patients should be screened for warning signs or complications associated with respiratory tract infections. Pharmacists and pharmacy staff should carry out a structured approach to each consultation to ensure each patient receives appropriate counselling, treatment and referral if necessary.
Prevention is important in reducing the spread of flu, with vaccination the best approach in preventing and reducing severity of symptoms. Hand hygiene and other measures can also be effective in reducing transmission of respiratory viruses. The diagnosis of cold and flu is generally based on symptoms and physical examination, with laboratory tests used only if necessary.
Antibiotics are not effective in treating cold and flu, and their use can lead to the development of antimicrobial resistance. Antimicrobial stewardship is a set of measures to counteract resistance and pharmacists have an important role in this process. Depending on the symptoms; analgesics, antihistamines, decongestants, antitussives and expectorants can be used to provide symptomatic relief. Non-pharmacological treatment and self-care can also play a role in the treatment of cold and flu. Antiviral treatment may be initiated within 48 hours of symptom onset in patients who are deemed to be at risk of complications.
Introduction and epidemiology
The common cold and flu are both upper respiratory tract illnesses caused by viral infections. They both tend to be acute, self-limiting and may sometimes involve the lower respiratory tract.1 Both the common cold and flu are contagious respiratory illnesses but are caused by different viruses; flu is caused by different influenza viruses and the common cold can be caused by coronaviruses, rhinoviruses, adenoviruses and parainfluenza viruses.1 The incidence of the common cold and flu is subject to seasonal variation, with a higher incidence in winter compared to summer. The common cold is the most common illness in the world, with an average of 6-8 episodes per year in children, decreasing to 2-4 episodes per year in adults. It can have a large economic burden due to absenteeism at work and school.2
Symptoms
The common cold and flu can share similarities in symptoms but difference exist between the viruses. The common cold generally has a gradual onset of symptoms, compared to the more sudden onset of flu symptoms, which usually appear within a few hours. Both viruses can be unpredictable, but symptoms generally start to resolve after one week. Symptom of cold are usually limited to the upper respiratory tract (nose and throat) and flu symptoms generally affect more than just the upper respiratory tract, with symptoms of flu usually much more severe than those of a cold. Symptoms of a cold can include blocked or runny nose, sneezing, cough, sore throat and fever.3 Symptoms of flu can include fever, fatigue, body aches, headache, difficulty sleeping, loss of appetite, dry cough and nausea. Runny nose and sore throat are also possible, but less common than with the common cold.4, 5 Influenza can be classified into uncomplicated and complicated. Uncomplicated flu is characterised by the sudden onset of the typical symptoms outlined above, with symptoms generally resolving in less than two weeks. Complicated flu occurs when the viral infection causes a potential wide range of complications that can result in severe disease.6
Complications and Warning Signs
The common cold and flu are generally self-limiting in healthy individuals and usually will resolve within two weeks. However, flu and complications of flu can lead to serious illness. In children, otitis media (middle ear infection) and respiratory complications including croup and bronchiolitis are most common. Rarer complications in children can include myocarditis, pericarditis, encephalopathy, encephalitis and Reye’s syndrome. The most common complications of flu in adults are pneumonia and bronchitis, which can lead to respiratory failure, acute respiratory distress syndrome, septic shock or multi-organ failure. Flu can often cause dehydration, which can exacerbate underlying chronic medical conditions.6 Patients that are aged 65 years or older, pregnant or have a longterm medical condition are at an increased risk of complications from flu. As patients with asthma, COPD, diabetes and heart failure are at a higher risk of complications, there may be a need to refer to a medical doctor for further treatment. Pharmacists and pharmacy staff should be aware that patients may need referral to a doctor if their symptoms don’t improve after 7 days or they have a weakened immune system, due to HIV or chemotherapy.7
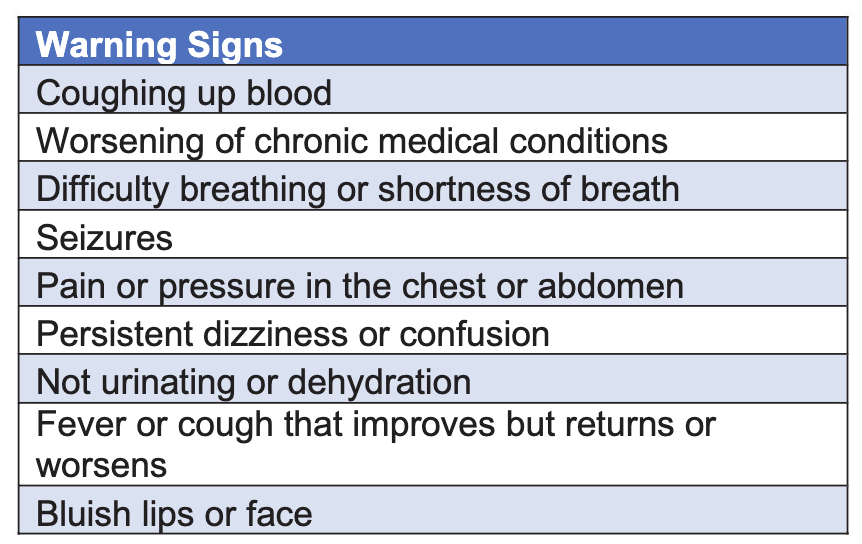
In the event of patients experiencing any warning sign symptoms, then they should seek medical attention immediately. Pharmacies are often the first port of call for patients with symptoms, pharmacy staff should recognise when referral is necessary. Some of the more common of these warning signs are outlined in the table on page 42.
Community Pharmacy Role in Cold and Flu
Community pharmacy is often the first port of call for patients when they have symptoms of cold or flu. Most symptoms can be effectively treated by using over the counter (OTC) medicines from community pharmacies, which can help reduce the burden on other primary care providers and emergency departments. A systematic approach to each consultation should be implemented to ensure a consistent high-level of care to each patient presenting with cold and flu symptoms. A patientcentred approach should be followed in community pharmacy. All pharmacy staff should be fully trained and competent in conducting OTC consultations. There is a great importance in tailoring each consultation to reflect the different role, responsibility and knowledge of the staff members. Pharmacy staff should know when to refer to the pharmacist when carrying out each consultation.9
Effective consultations between pharmacy staff and patients are fundamental to ensure appropriate recommendations are made and desired patient outcomes are achieved. Optimal management of these consultations require effective information gathering from the patient, with proper use of a framework essential for retrieving information. Who is the patient, What are the symptoms, How long has the patient had the symptoms, Action to date and other existing Medication being taken (WWHAM) is the most common framework used in information gathering. Effective communication skills are necessary to counsel each patient and communication style may be required to be tailored to each patient. Pharmacists should oversee consultations to ensure correct treatment options are selected or patients are referred if necessary.9
Antimicrobials and Antimicrobial Stewardship
Antimicrobial resistance (AMR) occurs when bacteria, viruses, fungi and parasites adapt over time and are no longer treatable by antimicrobials. This makes infections much more difficult to treat and increases the spread of disease, morbidity and mortality.10 Antibiotics are not effective in treating viral infections such as the common cold and influenza and therefore should not be used in the treatment of these illnesses. Overuse of antibiotics can lead to the development of antibiotic-resistant pathogens.11
Studies have estimated that approximately half of antibiotic use is either unnecessary or inappropriate. Therefore, there are major concerns about potential adverse effects from overuse of antibiotics, as well as the selection of antibiotic-resistant pathogens. The slowing of the development of new antimicrobials have left fewer treatment options for antibiotic- resistance pathogens, leading to an increase in duration of illness, hospital stay, cost, morbidity and mortality. Antibiotic resistance is a major threat and a concerted effort, including not prescribing antibiotics for cold & flu, must be made.
Antimicrobial stewardship is a set of measures that has the objective of improving the appropriate use of antimicrobials. It does this by ensuring the correct antimicrobial treatment is selected for the appropriate infection, as well as the correct duration of therapy, dosage and route of administration.14 Antimicrobial stewardship has been shown to reduce a pathogen’s resistance to antimicrobials without having a negative effect on clinical outcomes such as duration of illness, length of hospital stays, morbidity or mortality. Antimicrobial stewardship will also ensure a reduced risk in the development of superbugs.12
Pharmacists can play an important role in antimicrobial stewardship, particularly in the context of cold and flu. Encouraging hand hygiene techniques and vaccination reduces transmission of viral infections and therefore reduces inappropriate prescribing of antibiotics. Pharmacists can have discussions with prescribers about the inappropriate prescribing of antimicrobials for viral infections such as the common cold and flu. Pharmacists can mention the lack of effectiveness of antibiotics in treating cold and flu, with potential for adverse effects and development of antibiotic resistance. As drug experts, pharmacists can contribute to antimicrobial stewardship by influencing those crucial prescribing decisions. Pharmacists can discuss other treatment options with the prescriber that focus on symptomatic relief for the patient.15 The HSE have thorough guidelines on antibiotic prescribing for community infections that is very useful.16 Pharmacists are also ideally placed to counsel patients on the lack of effectiveness of antibiotics on viral infections and potential risks associated with their use. Pharmacists can effectively communicate to patients that these illnesses are generally self-limiting and symptomatic treatment can be much more useful that antibiotic treatment.15
Prevention
Prevention is key in reducing the burden of cold and flu in society. Pharmacists are trusted healthcare professionals and therefore can reshape patient perceptions and reinforce the messaging around prevention of infection. Vaccination is an important preventative measure against influenza. Unfortunately, due to many different serotypes of the common cold, it is not possible to vaccinate against this illness. Simple measures including regular handwashing with soap, avoiding touching the face and cleaning surfaces that people regularly touch can help prevent spread of respiratory viruses. Covering coughs and sneezes with a tissue and discarding the tissue immediately after use, improving ventilation in buildings and avoiding close contact with other people when symptomatic are all also practical measures that patients can be counselled on to reduce spread of common cold and flu.17, 18
Vaccination
Vaccination is the best method of protection against flu.19 Vaccines contain weakened or inactive parts of a pathogen that triggers an immune response in the body, that will produce antibodies and offer protection if exposed to the pathogen later.20 The flu vaccine should be administered annually as the antibodies reduce over time, as well as the fact that flu strains can change from year to year. The vaccine is generally available from October to April, but it is ideal to get it as early as possible, before the commencement of flu season. Vaccination generally reduces the risk of getting flu by 40% to 60% and can also reduce intensity and duration of symptoms. There are usually two vaccines available in Ireland; the quadrivalent influenza vaccine (QIV) which is generally used for over 18 years old and the live attenuated influenza vaccine (LAIV) which is used for those aged 2 to 17 years old.21 The preferred administration site for the QIV is in the deltoid muscle via intramuscular injection.22 The LAIV is administered nasally, with half of the dose administered via a spray in both nostrils.23 Mild side effects are possible and can include fever, fatigue, soreness or swelling at injection site, body aches and headaches. Nasal congestion is also common with nasal administration of the vaccine. These are generally self-limiting and will resolve within 48 hours. Taking paracetamol and resting are advised if these side effects are experienced. More serious side effects are rare and should be reported to the HPRA.
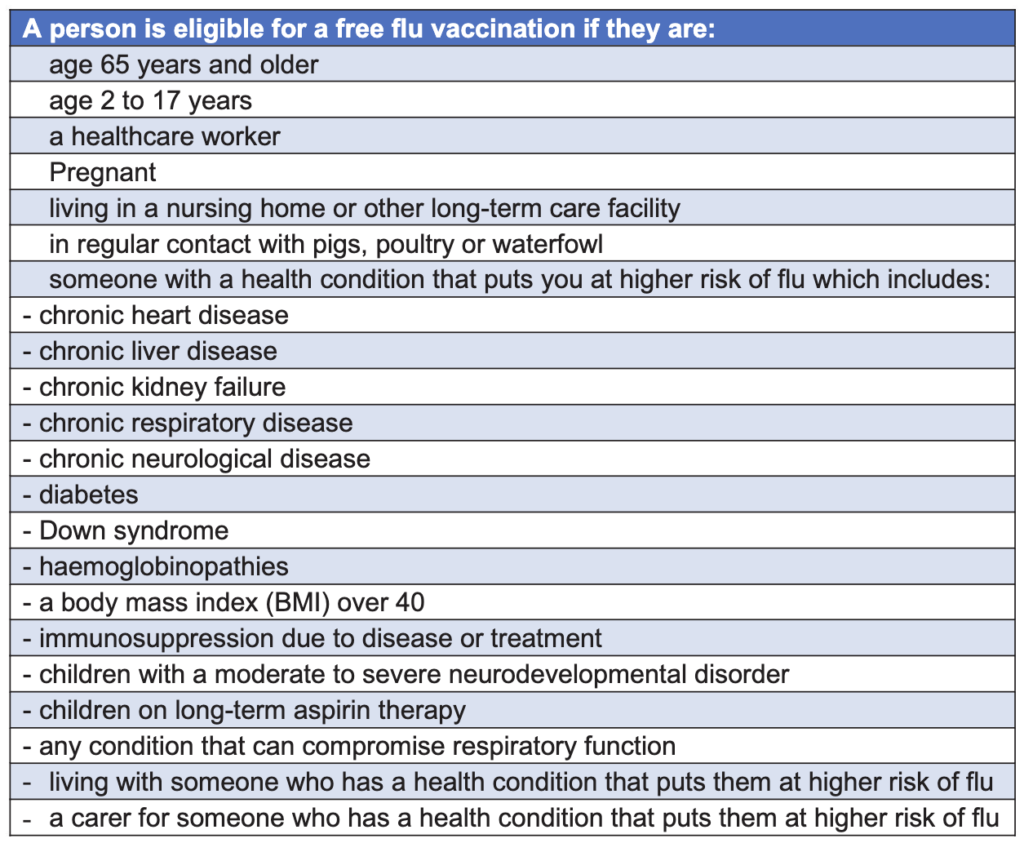
A wide number of people in Ireland are eligible for a free flu vaccination in Ireland and these are outlined in the table below.24
Pharmacists have been providing a seasonal influenza vaccination service in community pharmacies since 2011.25 Flu vaccination service in community pharmacies has been reported to improve uptake of the vaccine. Recommendations from healthcare workers have also shown to greatly improve vaccination rates. As patients visit their community pharmacy much more often than their primary care physician, pharmacists have a very important role in this. Pharmacist can counsel patients on the benefits of vaccination, risks of not getting vaccinated and ease patient concerns regarding potential side effects.26
Diagnosis
The diagnosis of common cold and flu is generally based on symptoms and physical examination. As these illnesses are usually self-limiting, symptoms can be examined by a physician and a diagnosis made without need for further diagnostic tools. Rapid influenza diagnostic tests (RIDTs) can be used to diagnose influenza by detecting antigens.
that stimulate an immune response. Molecular assays that detect genetic material of influenza can be used and are more accurate than RIDTs. Both tests take less than 20 minutes to perform. Specialised laboratory tests such as polymerase chain reaction (PCR) tests can be used for diagnosing influenza. These tests are usually not required but can be useful in differential diagnosis between common cold, influenza and other respiratory infections including Covid-19. Reliability can be an issue for all these methods of diagnosing.28 Therefore, diagnostic tools are not very useful, and treatment can be initiated if required based on clinical symptoms, patient history and physical examination.29
Treatment
Treating based on symptoms that a patient exhibits is the mainstay of treating common cold and flu. Getting a full knowledge of clinical symptoms and patient history is important in selecting an appropriate treatment option. OTC analgesic options including paracetamol and ibuprofen are useful in treating aches and pains, as well as lowering fever associated with the viral infection.30
Antihistamine
First-generation antihistamines such as brompheniramine and chlorpheniramine have been shown to provide some symptomatic relief. This involves a reduction in symptoms such as sneezing and nasal discharge, as well as a reducing the duration of symptoms. Side effects associated with diphenhydramine include drowsiness, dry mouth and blurred vision.31 Second-generation antihistamines are ineffective in treating symptoms of cold and flu.32
Decongestant
Decongestants have been shown to have clinical effectiveness in reducing symptoms of rhinorrhoea, nasal congestion and sneezing.31 Pseudoephedrine and Phenylephrine are two decongestants that are licensed for OTC use in those aged 12 years and older in Ireland. Potential side effects can include agitation, hypertension, tachycardia, nausea and dysrhythmia. Decongestants can also be used in combination with a first-generation oral antihistamine. Xylometazoline is a decongestant that can be used topically to reduce nasal symptoms. Side effects of nasal decongestants can include irritation of nasal membranes, rebound congestion and nosebleeds.31
Cough medicines
Codeine is an opioid antitussive and used to be the gold standard treatment for cough. It is no longer recommended due to lack of evidence of efficacy and many side effects associated with its use including dependence, drowsiness and constipation.
Dextromethorphan is a non-opioid antitussive and does have efficacy in suppressing cough caused by upper respiratory tract infections31 Expectorants and mucolytics have efficacy in treating productive cough caused by acute upper respiratory tract infections. They work by increasing the volume of sputum in the airway and decreasing the viscosity, which promotes effective clearance of mucus. Clinical studies have shown the efficacy of expectorants in treating acute upper respiratory tract infections, where excess mucus and cough are symptoms34 Carbocisteine (from 2 years and older) and guaifenesin (from 6 years and older) are available OTC in Ireland.35, 36
Non-pharmacological treatment
Daily administration of zinc has effectiveness in reducing the number of colds per year, particularly in children. Other supplements such as vitamin C, vitamin D and garlic have mixed results, with studies showing no benefit versus placebo. Natural products including ginseng and echinacea showed no clear evidence of benefit. Homeopathy also does not have a positive effect on preventing or treating the common cold or flu.37 Honey may be useful in treating nighttime cough in children but should not be used in children under 12 months due to the risk of infant botulism. Bulb suction with saline drops can be useful in relieving nasal symptoms in children. Vapour rub containing ingredients such as eucalyptus, camphor and levomenthol may provide symptomatic relief in children over 2 years old.
Self-Care
Pharmacists and pharmacy staff should ensure patients are counselled on the importance of self-care in the treatment of cold and flu. Patients should be advised to keep warm, avoid smoking and eat well. Getting plenty of rest and sleep are important in self-care treatment, with the patient advised not to return to normal activities until they feel well enough to do so. Patients should be counselled to drink plenty of water as dehydration can lead to complications. Urine should be a light yellow or clear colour.3
Antiviral treatment
Flu can also be treated orally with Oseltamivir (Tamiflu) and by inhalation with Zanamivir (Relenza). These are both antivirals of the neuraminidase inhibitor class, which have activity against both influenza A and B. Previously healthy patients with no underlying condition generally do not need antiviral therapy, unless the clinician feels the patient is at risk of developing complications. Symptomatic treatment is generally recommended for these patients. Patients who are deemed to be at risk of complications should be commenced on Oseltamivir as soon as possible, even without laboratory confirmation of diagnosis. Oseltamivir is also recommended for treating flu in pregnancy due to potential adverse clinical outcomes for this patient group. Initiating antiviral treatment within 48 hours of symptom onset can reduce risk of complications including pneumonia and respiratory failure. It can also reduce risk of hospitalisation, morbidity and mortality.39
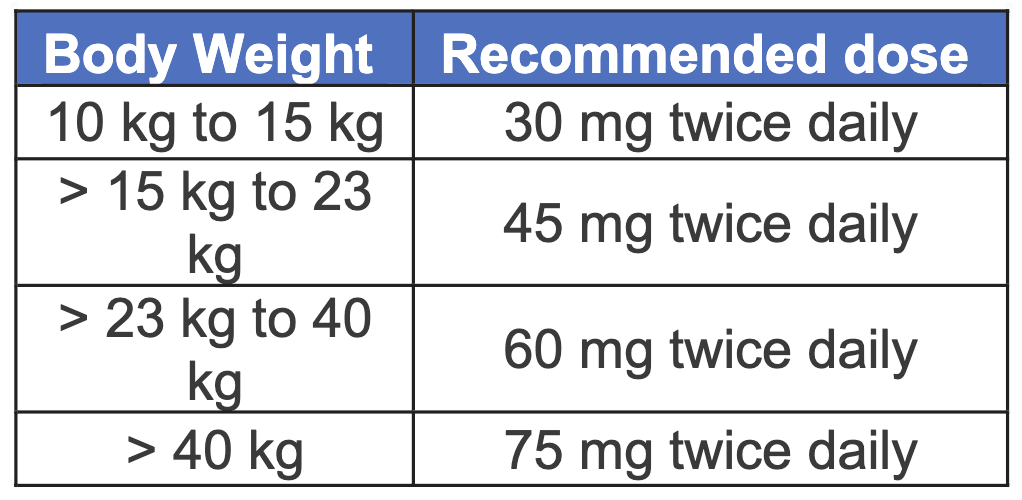
The recommended treatment dose of Oseltamivir is 75mg twice daily for adults and adolescents aged 13 years and over, with a body weight of greater than 40kg (see table left). In infants and children aged from 1-12 years, the weight-adjusted dosing regimen outlined in the table below is recommended.
3 mg/kg twice daily is the recommended dose for infants 0 – 12 months of age. However, this dosing regimen is not suitable for infants with a post-conceptual age less than 36 weeks.40 of treatment is usually 5 days, with 10 days for oseltamivir in immunocompromised adults and adolescents recommended.
If oseltamivir resistance is suspected, zanamivir can be initiated within 48 hours of symptom onset. The recommended dose is 10mg (2 inhalations) every 12 hours. The product is authorised for use in the EU but as it is not marketed in Ireland, it is only available as an unlicensed product. Specialised advice should be sought if considering initiating zanamivir.39 References available on request
AUTHOR: Donna Cosgrove PhD MPSI
Donna graduated with a BSc in Pharmacy from the Royal College of Surgeons in Ireland. She then returned to university to complete a MSc in Neuropharmacology. This led to a PhD investigating the genetics of schizophrenia, followed by a postdoctoral research position in the same area. Currently Donna works as a pharmacist in Galway, and as a clinical writer.
Read more from IPN November Here
Read more CPD Here