Every year, suicide accounts for over 800,000 deaths globally. Every life lost represents someone’s partner, child, parent, friend or colleague.
Pharmacists have regular contact with customers who may be suicidal. In recent years, the role of pharmacists has changed. They increasingly offer both advice and
consultations to the public. Many pharmacists become familiar with regular customers and, as a result, may be better placed to identify deteriorations in their mental state.
It is essential that pharmacists become more involved in the care of mental health service users. Systems could be developed to inform pharmacists of those who are at high risk of suicide, such as those who have previously attempted suicide. Pharmacists could remain particularly vigilant over such individuals and prompt appropriate discussions around the topic by suitably trained professionals.
Suicide Strategy Ireland
In November of last year, the Minister for Health, Stephen Donnelly TD and the Minister of State for Mental Health and Older People, Mary Butler TD, announced the extension of Connecting for Life, Ireland’s National Strategy to Reduce Suicide, to 2024.
The extension will allow for:
• continuation of the Cross-Sectoral Connecting for Life Implementation Steering Group, for senior leadership and oversight of the Strategy. The Group is chaired by
the Department of Health, with representation from 12 government departments, the HSE, Tusla and two NGOs
• a continued co-ordination and implementation role for the HSE National Office for Suicide Prevention (NOSP), with a current budget of €13 million per annum
The extension of Connecting for Life now provides an opportunity to further advance and embed many already-established local Connecting for Life implementation structures throughout the country. The 17 local Connecting for Life Action Plans that are already in place, will in turn be extended and updated to reflect a new national implementation plan.
National implementation
structures, most notably the National Cross Sectoral Steering and Implementation Group, will continue to coordinate different government departments and (departmental) strategies. The HSE National Office for Suicide Prevention (NOSP) remains the named provider of cross-sectoral support for implementation of Connecting for Life.
The NOSP has now published a new and responsive implementation plan for 2020 to 2022, which is rooted in the principle of learning from previous experience of implementation to date. Specifically, this plan has been informed by the findings of the 2019 independent Interim Strategy Review of the implementation of the strategy, and consistent consultation with implementation partners, stakeholders and government departments.
In this article, we take a brief look at the Implementation Plan.
Connecting for Life
The main aim of CfL is to reduce suicide in Ireland, with a 10% reduction in suicide rates adopted as the minimum target of the strategy. This target was set by the World Health Organisation (WHO). Given the complex and multifarious nature of risk factors for suicide, achieving this target will be challenging, and as the interim review of CfL highlighted, so too will be evidencing the contribution of CfL to any reductions observed.
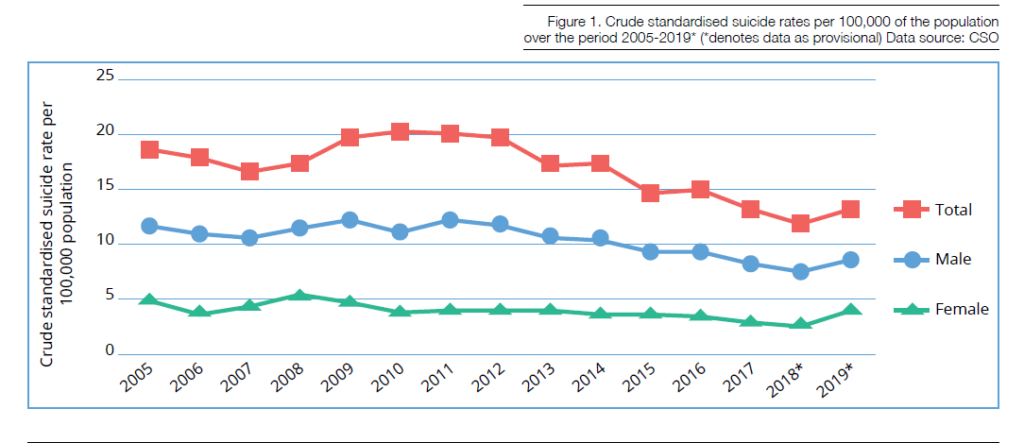
Figure 1 illustrates the trends observed in suicide rates in Ireland over the period 2005-2019. Analysis of the crude standardised suicide rates indicates that there was a substantial increase in suicide rates observed during the recession years in 2009-2013, followed by successive decreases during the 2015-2018 period.
Looking at the period covered in figure 1, the male rate is approximately 4 times higher than that of females, with this lowering to approximately 3 times higher in 2019. Provisional data indicates an increase in suicide rates observed in 2019 for both men and women, however caution is required in interpreting the 2018 and 2019 data as it is not yet finalised.
The increase observed in both the provisional suicide rate and selfharm rate in recent years highlights the need for a continued focus on the systematic implementation of CfL and importance of timely data to inform decision making throughout the lifetime of the strategy. However, there are a number of issues with suicide data in Ireland presently that NOSP is planning to address over the lifespan of this second implementation plan, namely: Getting more timely data on suicides in Ireland and; Getting
more accurate and comprehensive data on those that die by suicide.
In CfL 2015-2020 there was an identified list of priority groups for suicide prevention activities. These groups were as follows:
• health/mental health related groups: People with mental health problems of all ages, those who have engaged in repeated acts of self-harm, people with alcohol and drug problems and people with chronic physical health conditions;
• minority groups: Members of the LGBTI+ community, members of the Traveller community, people who are homeless, people who come in contact with the criminal justice system (e.g. prisoners), people who have experienced domestic, clerical, institutional, sexual or physical abuse, asylum seekers, refugees, migrants and sex workers;
• demographic cohorts: Middle aged men and women, young people and economically disadvantaged people;
• suicide related: People bereaved by suicide;
• occupational groups: Healthcare professionals, professionals working in isolation, (e.g. veterinarians, farmers).
For phase two of CfL, it is planned to revisit the current list of priority groups, following a comprehensive internal review in NOSP to identify gaps, and to determine a more focused, strategic approach to working with priority groups for phase two of the strategy. This is based on one of the recommendations of the interim review of the strategy which called for the development of a strategic plan to inform CfL activity intended to prevent suicidal behaviour among priority groups.
Impact of Covid-19
It is likely that the Covid-19 pandemic will impact on mental health, and this has been indicated in findings from the Covid-19 Psychological Response Consortium (C19PRC) study – a collaboration between researchers in Ireland, Spain and the United Kingdom.
Initial findings from this study (which surveyed approximately 1,000 respondents in Ireland) reported that mental health problems are common; 41% of people reported feeling lonely, 23% reported clinically meaningful levels of depression, 20% reported clinically meaningful levels of anxiety, and 18% reported clinically meaningful levels of post-traumatic stress (Hyland and Daly, 2020).
NOSP successfully submitted a proposal to this Consortium requesting that questions on suicide are added to the standardised survey for this study, which will be administered monthly during the course of the Covid-19 pandemic period.
This will provide useful, timely data on the impact of Covid-19 on mental health and suicidal ideation in particular.
The emerging impact of Covid-19 on the work of CfL NGO partners has also been evident in monthly surveys conducted to track the effects of the public health emergency on their suicide prevention work. While it has been apparent that NGO partners have adapted effectively to the demands placed in them by Covid-19, there have been some concerns.
NOSP plans to use data from the C19PRC study and regular surveys to track the impact of Covid-19 on mental health and inform suicide prevention work in phase two.
Sharing the Vision
Launched in June 2020, ‘Sharing the Vision – A Mental Health Policy for Everyone’ is the successor to ‘A Vision for Change’ that was launched in 2006. Sharing the Vision focuses on developing a broad based, whole system mental health policy for the whole of the population. The vision of the policy is to create a mental health system that addresses the needs of the population through a focus on the requirements of the individual.
This mental health system should deliver a range of integrated activities to promote positive mental health in the community. It should intervene early when problems develop; and it should enhance the inclusion and recovery of people who have complex mental health difficulties. Service providers should work in partnership with service users and their families to facilitate recovery and reintegration through the provision of accessible, comprehensive and community based mental health services.
This policy supports continued implementation of Connecting for Life and specifically states that the Department of Health will extend the timeframe and funding for CfL to 2024.
Specific actions which overlap with CfL (and, in particular, this implementation plan) can be seen in the areas of: stigma reduction; mental health promotion; whole school wellbeing promotion; improved pathways of care; social prescribing; enhanced access to talk therapies, dual diagnosis; enhancement of the National Clinical Care Programme for the Assessment and Management of Patients Presenting to emergency departments following self-harm; the priority groups of homeless people, those in direct provision, travellers and prisoners; and better suicide data.
Membership of Steering Committee
The membership of the National Implementation and Monitoring Committee (NIMC) Steering Committee has been announced, to implement Sharing the Vision.
• Mr John Saunders (Chair)
• Ms Fiona Coyle, Advocacy Expert
• Ms Aisling Culhane, Psychiatric Nurse
• Ms Kerry Cuskelly, Social Worker
• Mr Maurice Dillon, Occupational Therapist
• Dr Joseph Duffy, Psychologist and Youth Mental Health Services Lead
• Dr Daniel Flynn, Psychologist
• Dr Siobhan MacHale, Psychiatrist
• Mr Dave Maguire, Department of Health Lead
• Mr John Meehan, HSE
• Dr Amir Niazi, HSE National Clinical Lead
• Dr Brian Osborne, GP
• Ms Caroline Pigott, Department of Health Sláintecare Lead
• Mr Ian Power, Youth Mental Health Expert
• Mr Jim Ryan, HSE
• Mr Michael Ryan, HSE Mental Health Engagement
• Dr Anne Marie Waldron, Psychiatrist (CAMHS)










