The Irish Patients Association, founded as Ireland’s first independent, cross-disease patient advocacy group, operates on a non-political basis with a focus on patient safety and rights protection. Since 2013, the association has been reliant on voluntary work without public funding from the Health Service Executive (HSE) or paid staff.
Patient safety in Ireland’s healthcare system remains fraught with issues, including problems within Emergency Departments, prolonged waiting times for consultant appointments and surgeries, restricted access to GP panels in various regions, and persistent funding overruns. While some issues are due to resource limitations, others require cultural and operational changes rather than just financial input. A critical area for improvement is the corporate conduct towards patients, which often lacks the expected standards of respect and professionalism. Corporate conduct encompasses how healthcare organizations interact with patients, manage medical errors, allocate resources, and ensure transparency and responsiveness in addressing patient concerns and complaints.
Financial Concerns Amid Workforce Issues
The HSE has secured a ¤1.5 billion supplemental budget to manage this year’s overspending, aiming to mitigate any adverse impacts on patients. However, there is concern regarding the HSE’s workforce cap of 130,000 by the end of 2024, which is significantly lower than the current annual turnover rate of 145,985 WTE or 163,792 personnel. Clarity on this cap is necessary to ensure adequate staffing levels to meet patient needs. Furthermore, the unresolved Internal Audit investigation into the ¤19 million intended for children’s spinal operations raises additional concerns. The HSE’s approach needs to transition from a reactive to a proactive stance, identifying and addressing issues before they escalate.
Patient User Experience
The HSE own Patient Experience Survey conducted by HIQA for 2022 reports high satisfaction levels however Patients were also less positive about the availability of emotional support, time to discuss care and treatment with a Doctor, information on how to manage a condition after leaving hospital, and opportunities for family members to talk to a Doctor.
22% of participants said that they did not find a member of staff to talk to about their worries and fears.
On the other hand, benchmarking against other industries presents a different insight.
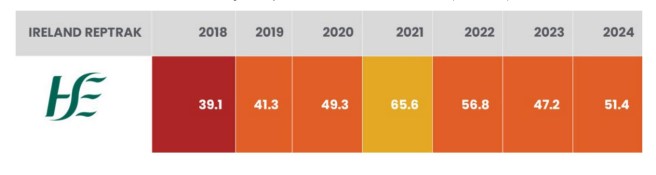
In May 2024, the strategic communications firm, The Reputations Agency, published its Ireland RepTrak® 2024 report which studies public perceptions of 100 of the largest, most important and most familiar organisations in Ireland. This year the HSE, with an annual budget of ¤23Billion, was positioned in the weak reputation tier and ranked in 95th place. The challenge for the HSE is to understand why they have performed in this way compared to for example the Mater Private Network and the Blackrock Healthcare Group who ranked in 7th and 10th position respectively in the same study.
[See table 3.]
Patient Experiences Reflect Systemic Issues
Several patient experiences in 2024 highlight systemic failures requiring urgent attention. Issues include poor communication and unprofessional behaviour from healthcare providers. For instance, patients have reported being told that there are “sicker people” who need attention or that management prioritises other issues over their concerns, which is disrespectful and unprofessional.
Examples of Problematic Conduct Include:
Handling Phone Calls: One patient’s calls to Hospital A were redirected to Hospital B, resulting in a curt response and a disconnected line when attempting to proceed with a transfer request.
Mixed Wards: An elderly patient was repeatedly placed in mixed wards against her will and preferences, allegedly due to discriminatory practices favoring certain patients for private or female-only wards.
Long Waits and Communication: The extended wait for ADHD assessments has left patients in limbo for over a year without clear timelines, significantly impacting their well-being.
Surgical and Equipment Failures: Last-minute cancellations of surgeries due to overlooked health issues and denial of necessary
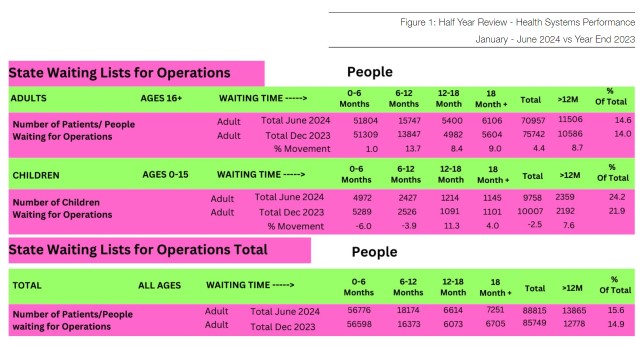
Figure 2: Disparities in Consultant Waiting Times

medical equipment for home discharge demonstrate a lack of thoroughness and disregard for patient needs.
Challenges in Care Transfer and Delayed Diagnoses
Patients also face difficulties in transferring care closer to home. One patient, who had traveled extensively for 20 years, struggled to switch to a more conveniently located hospital due to new waiting lists, despite serious conditions. This highlights systemic issues in patient management and accessibility. Additionally, delayed diagnoses and dismissive responses to patient complaints further tarnish the healthcare experience. For instance, a patient’s injury was ignored for months, and when accountability was sought, the response from the Doctor was irritated and dismissive.
“Change and Reform in our healthcare systems should not be preceded by preventable funerals and injury to patients”
Waiting Lists and Cancellations
Waiting lists for operations are growing, with adult lists increasing by 4.4% by Q2 2024 compared to the previous year. The number of patients waiting 6-12 months, 12-18 months, and over 18 months has also risen. For children aged 0-15 years,
waiting lists grew by 28,000 in the first 16 weeks of 2024, despite a minor overall drop. Misallocation of ¤19 million intended to reduce waiting times and improve spinal and orthopaedic services for children underscores the need for accountability and effective fund management. The Department of Health has requested an audit of children’s orthopaedic care to examine the use of this funding.
Cancelled Operations and Overcrowded Emergency Departments
Overcrowding in emergency departments led to 50,000 operation cancellations in the first quarter of 2024, which could have reduced the waiting list by 55%. This overcrowding significantly impacts patient safety and highlights issues in capacity and processing efficiency within the HSE. The HSE should adopt best practices, including detailed reporting on rescheduled operations post-cancellation, similar to the NHS in England.
Disparities in Consultant Waiting Times
As of mid-2024, 20.5% of the population without private health insurance is waiting for their first consultation with a hospital
consultant, whereas those with private insurance face minimal waiting times. This disparity raises concerns about the effectiveness of Sláintecare, especially if unsafe waiting times are not reduced significantly. While there has been a 5% decrease in patients waiting over 18 months, the number waiting between 12 and 18 months has surged by 17.7%. Alarmingly, children are now experiencing longer waits than adults, with 16.1% of children waiting over 12 months by June 2024 compared to 14.2% at the end of the previous year.
Conclusion: The Importance of Conduct
The Importance of ConductThe Reputations Agency Ireland RepTrak® 2024 report highlights that conduct is as crucial as products and services in building and protecting reputations. Healthcare organisations must prioritise fairness, transparency, and ethical behaviour to uphold patient rights and improve care quality. A commitment to respectful and compassionate interactions with patients and their carers is essential. This commitment is vital in a financially constrained yet hungry industry and starts with genuinely listening to patients and their families.
Figure 3: Table 3 HSE scores over the past seven years