Written by Elaine Buckley and Edward Murphy, HSE Tobacco Free Ireland Programme
Background
Each year in Ireland, over 4,500 people die due to smoking. Each day across our hospitals, one in five people with respiratory disease, one in eight people with cancer and one in ten people with circulatory disease are admitted because of smoking-related harm. People who smoke are almost twice as likely to have a chronic illness compared to those who don’t smoke, and each day require support from our primary and community care services.1
These numbers are a stark reminder that Ireland is still experiencing an epidemic of smoking-related harm. Behind these numbers are real people. Our relatives, friends, colleagues and loved ones who experience disease, disability and sadly die prematurely because of smoking. Even more heart breaking is the fact that the suffering caused by smoking is completely avoidable.
Thankfully, smoking in Ireland is now less common than it was in the past. We have all worked hard collectively to build a society where smoking is no longer a social norm. The benefits of this are visible in the fewer numbers of younger people who now smoke.
In November, The Healthy Ireland Survey2 reported that 18% of the Irish population currently smoke (down from 23% in 2015). Those aged 25-34 remain the most likely age group to smoke (22%). Men (21%) remain more likely to smoke than women (15%). Smoking rates are higher for those who are unemployed (40%) than those in employment (17%).
The Healthy Ireland Survey also indicates that many of those people who smoke want to quit. 33% of people who smoke are either trying to quit or actively planning to do so. 49% of those have smoked in the past year have attempted to quit, with 23% of this group successfully quitting.
How can you support people to stop smoking?
Effective stop smoking care is now well established and the World Health Organisation has described Ireland’s efforts as representing the ’Gold standard’ in this area.
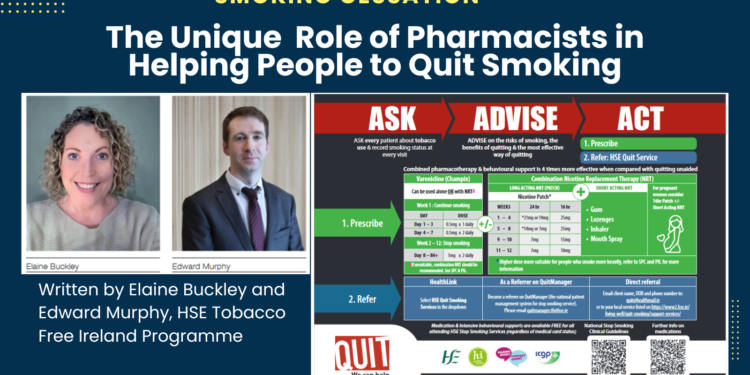
In January 2022, the Department of Health published Ireland’s first National Stop Smoking Clinical Guidelines.3 The Pharmaceutical Society of Ireland was represented on the Guideline Development Group throughout the guideline formulation process. These National Stop Smoking Clinical Guidelines aim to:
1. Define good clinical care for people who smoke across a range of settings, regarding the management of smoking cessation among the general adult population. They also have a special focus on the care that should be provided to women who are pregnant and users of secondary mental health services.
2. Recommend that healthcare professionals routinely
ASK people about their smoking, ADVISE them to stop and provide or ACT by 1) Recommending or prescribing stop smoking medication and 2) Referring to QUIT Services
These 3 steps when delivered routinely in care can increase the chance that someone will quit and remain smoke-free by 2 to 3 fold.
3. Set out the recommended behavioural and pharmacological supports that can support people who smoke to quit.
Nicotine plasma concentration time profiles following smoking and NRT

The unique and influential role of pharmacists in helping people to quit
Healthcare professionals, particularly pharmacists, have a unique expertise and opportunity to promote correct and sustained use of stop smoking medications and refer to local HSE stop smoking services for behavioural support.
All stop smoking medicines work best when combined with behavioural support from a certified stop smoking advisor. HSE Stop Smoking Advisors who deliver the quality assured and evidence based standard treatment programme to clients who wish to quit smoking, recommend combination Nicotine Replacement Therapy (NRT) based on the clients nicotine dependence sore (long acting product) and client choice (short acting product). The single biggest mistake with NRT is under-dosing as undertreated cravings increase the risk of smoking relapse. We know NRT also has a role to play where there is a short-term need to quit smoking e.g. when traveling by airplane. Pharmacists can further support the client on their quit journey by providing additional information on a range of NRT including patches, gums, lozenges, sprays, and inhalers.
The National Stop Smoking Clinical Guidelines recommend combination nicotine replacement therapy i.e. a slow-release patch should be used in combination with a fast acting product, such as gum or mouth spray. Varenicline (Champix) can be added to combination nicotine replacement therapy when manufacturers make this available again. All of the NRT formulations produce relatively low levels of nicotine that contrast with the spikes of nicotine produced by cigarette smoking. Combining a nicotine patch with a rapid delivery form of NRT such as the nasal spray has been reported to be more effective than using a single type of NRT. Nicotine spray or inhaler can be used in combination with the patches to control breakthrough cravings.
It is generally recommended that NRT products are used by the client for up to 12 weeks. With combination NRT, the initial patch strength is determined by the amount smoked per day, lighter smokers can start on step 2 for example (14mg/24 hr patch or 15mg/16 hr patch). The 24hour patch is helpful if the client struggles with early morning cravings and the 16-hour patch is helpful for patients with sleep disturbances. For long acting and short acting products, the client should be supported to titrate their NRT over the 12-week course.
All healthcare professionals should advise pregnant women who currently smoke about the harms of smoking and the benefits of quitting. NRT can be recommended in shared decision-making following discussion of benefits and risks.
By asking a few quick questions about your client’s smoking habits and lifestyle, you can help to choose the product and strength best suited to their needs.
Some clients may express concern that using NRT is just like swapping one addiction for another, but this is not true. Smoking is highly addictive. As a drug delivery system, no other drug doses at such a high frequency.
Trained stop smoking advisors can assess a client’s nicotine dependence and provide advice on which treatment options suit best as well as working with the client over a 12-month period to support the behavioural elements of a quit attempt, examining in detail the clients psychological and emotional dependence on smoking and working with them to overcome this.
Remind your clients of both the immediate and long-term health benefits of stopping smoking
• After 8 hours, oxygen levels rise in the blood, and nicotine and carbon monoxide levels reduce
• After 48 hours sense of smell and taste improve
• After 3 days breathing gets easier and lung capacity increases


• Within 2-3 months lung capacity may increase by up to 30%. Blood flows more easily to the arms and legs
• Within 1 year, the risk of sudden death from a heart attack falls by half.
• Within 5 years the risk of smoking-related cancers will be greatly reduced
Electronic referral to QUIT services
You can now send electronic referrals to the HSE Stop Smoking services (QUIT) by selecting HSE QUIT Smoking Services from the Hospital drop down list in either Healthlink Online or your Practice Management System.
What we offer: Evidence based stop smoking support
A Standard Treatment Programme within the HSE Stop Smoking Service includes:
• Intensive behavioural support, an assessment of nicotine dependence ± advice on recommended pharmacological support
• A number of stop smoking consultations – pre quit consultation X 2, Quit date consultation, follow-up consultation at week 1, week 2, week 3, week 4, 12-week, and 52-week follow up
• FREE confidential, non-judgemental, professional support
• Access to FREE NRT through a local community pharmacy regardless of medical card status
• Face-to-Face, individual or group support, virtually or in local communities & hospitals
• Online supports on QUIT.ie (a personalised online QUIT plan, regular email and text message support)
Contact your local stop smoking services
The HSE provides local stop smoking clinics nationwide. The locations and contact details for individual clinics can be found on Quit.ie under ‘Stop Smoking Clinics’.
Call the QUIT team on Freephone 1800 201 203
References
1. The State of Tobacco Control in Ireland (2022), Second Report. HSE Tobacco Free Ireland Programme
2. Healthy Ireland Survey 2023 Summary Report. Department of Health.
3. National Clinical Guideline No. 28: Stop Smoking (2022). Department of Health.