You could ask many people who treat patients with Osteoporosis/ Osteopenia what they think should be the first line to treat those with bone loss and they would all give different answers. Every patient should be individually assessed to see which is the most appropriate treatment for them, as there are so many causes of this Silent disease. If you asked who should be treated for bone loss you will also get different answers. Those who want to be proactive about their bone health are now being discouraged. Most people who have experienced fragility fractures, or watched their loved ones suffer horrendously from untreated bone loss, are much more proactive about their bone health.
Have you ever heard of people being discouraged of ensuring that they do not develop or have a disease that has no signs or symptoms, that is known worldwide as the “Silent Killer” and is preventable in most people?
Have you ever heard of a patient under 60 with cancer not be given a first round, never mind a second round of Chemotherapy or Radiation, or not referred for a bone scan to screen for cancer due to the horrendous side effects from these treatments or radiation exposure?
The answer we would assume is NO. Why? It would be considered by many to be unethical. With bone loss, not to treat a person with a treatable disease, leaves them at risk of becoming disfigured, loss of their independence and dying prematurely. Like all medications the long term use of them legally have to be monitored and those who do not fit the typical older Osteoporosis patient profile should not be discarded and refused treatment, as this will increase their cortisol levels, which will further increase their fracture risk.
NOTE: Research shows that most fractures happen in the moderate to marked Osteopenia range, which is why the IOS (Irish Osteoporosis Society) still use these terms, as there is a significant difference in risk of fracture from a person having mild Osteopenia versus marked Osteopenia. Osteopenia is the early stage of osteoporosis, and a bone health plan should be initiated right away.
There are not many treatments for bone loss, but we all know the long term effects if a person is continually on steroids. This is why it is essential that no matter what age a person is (children are not included in this statement), they should be put on a bone health plan to prevent fractures occurring or recurring in the first place.
What we do know is that if we do not treat those with bone loss pre 60 years, these patients are at risk for the horrific secondary consequences of fractures, which lead to disfigurement, loss of independence and premature death. A woman in Ireland committed suicide and left a note saying that she could no longer live with the pain of multiple fractures. We are not a third world country, and no one should ever be placed in a position like this ever again.
A survey done last year by Athena pharmaceuticals of Irish men and women aged 40 to 90 years of age, found that 1 in 5 adults have fractured a bone since turning 40 years of age. Over one third of those surveyed reported they had fragility fractures, and the rate of fragility fractures was highest among the 40–54-year-old age group, which would have been expected in the older age groups.
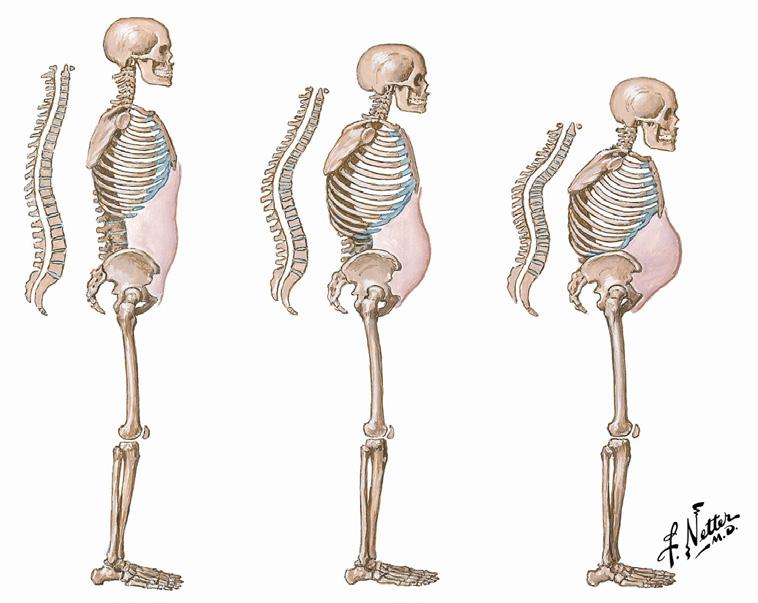
Vertebral wedge fractures result in a dowager’s hump, leaving a person disfigured and in pain and will significantly affect a person’s quality of life. Most lose the ability to be intimate with their partners, have low self-esteem, their ability to eat and drink can be affected, depending on how far forward their head is protruding, their ability to wash and dress themselves and actually live independently is taken away from them. It also leaves them at risk for mental health issues such as depression, anxiety and usually leads to isolation as they are embarrassed that they no longer look “normal”.
The significant damage to their vertebrae and rib cage, puts pressure on the intestines and bladder, leading to incontinence. The dowagers hump alters their centre of gravity, which places them at high risk of falling and encountering further fractures. They have difficulty buying clothing as their body shape has changed, and most women no longer can wear a bra. The rib cage is in contact with the pelvis; therefore, they have trouble reaching items higher than shoulder height or below hip level from kitchen cupboards etc.
We believe that not investigating and treating those under 60 who have had fragility fractures or are high risk for them, is playing “Russian roulette” with their lives, due to the secondary effects of fractures, many may not survive till 60 to be treated.
Unlike most treatments for other diseases, which people are taking to slow down the progression of the disease or to calm down the symptoms of the disease, Osteoporosis treatments have been proven to reduce fracture risk.
Those with a Dowager’s hump due to undiagnosed osteoporotic fractures are easily identifiable. It is those who have multiple risk factors for bone loss and undiagnosed bone loss who have not fractured yet, who should be referred for DXA scans to prevent them ending up disfigured and a burden on the health system.
A person can look perfectly healthy on the outside and have severe bone loss on the inside and the most cost-efficient way of knowing, is by getting a base line DXA scan, which costs approximately ¤120. A misconception is that a DXA scan has very high amounts of radiation, when it has 10% radiation of a regular chest X-ray. If a person has flown from Dublin to New York, they will have been exposed to more radiation than having a DXA scan done.
Bone markers are a way of checking to see how much bone is being lost and how much bone is being formed, however these tests are not cheap, and many GPS do not have access to request them, which is why a DXA scan, which is the world standard for measuring bone density should be one of the tools used to screen and diagnose people.
Considering 50% of women and 25% of men will develop bone loss, there should be a screening programme in Ireland for women and access for men at high risk to fracture, but it should not be based on age. It should be based on clinical judgment by the treating physician/s. We are all aware that women over 65 are the highest risk group for bone loss, due to having smaller bones and having gone through the menopause, however more men die from the complications of Osteoporotic fractures than develop prostate cancer.
There are some individuals who believe that due to the limited number of prescribed treatments for bone loss, treatment initiation to prevent fractures should not be initiated in younger age groups, unless they have had multiple fractures. Lately a prescription for vitamin D appears to be the most common treatment they are offered. The issue with this is, that sadly many of them will possibly end up in agony, lose their independence and not actually survive to be put on an Osteoporosis treatment.
Bone loss occurs leading up to the menopause, during the menopause, and significant boneloss can occur up to ten years post menopause. In an ideal world, every woman should have a DXA scan when they start to lose their periods heading into the menopause. This way if it shows the person already has lost bone, they can be put on a bone health plan, to build up their bone strength to help protect themselves, whilst going through the menopause. If they have good bone density, a plan can be put in place to help prevent bone loss.
NOTE: This type of strategy could save our health service a fortune long term as the cost of treating fractures in Ireland (those diagnosed) are shocking. The inpatient cost of just treating hip fractures in Ireland from 2014 to 2020 was 296 million and its rising.
Some women lose up to 30% of the overall bone in their body, when going through the menopause. This is why if a person has risk factors for bone loss, no matter what age, they should be referred for a DXA scan, as prevention is much cheaper and less painful, than treating fractures. It would be prudent to think about a national screening programme for women, similar to breast check considering 1 in 2 women will develop this Silent killer. 1 in 7 women will get breast cancer and all women are offered this screening service. Women have smaller bones and experience more changes in hormone levels, especially following menopause which is why they are more at risk than men.
Mammograms contain a similar amount of radiation as DXA scans, yet no one is talking about cancelling the National Breast Screening programme. The HSE initiated a DXA scan referral for GP’s, which should be encouraged, as DXA scanning is the world standard for screening/ diagnosing bone loss. With breast cancer, thankfully in many cases, symptoms such as lumps etc develop, but with Osteoporosis, there are no signs or symptoms until the person fractures.
Osteoporosis is one of the commonest diseases worldwide and hospital inpatient bed days, secondary to fractures are increasing. Research has shown that most fractures are preventable, which is why prevention of fractures in the first place, should be a major, logical priority. The fact a patient in their 30’s with severe Osteoporosis in their spine was told by a consultant, when the patient raised concerns that his bone density was continuing to decline on his DXA reports “Come back to me when you fracture” is shocking, but sadly is becoming more common. Would they allow their loved ones to fracture? For every 1 standard deviation decrease in BMD, the relative risk of fracture is significantly increased.
Those who have fought to survive cancer, should not end up disfigured, have loss of self-esteem and the secondary effects that occur from becoming deformed, because they are not 60+. It is much cheaper to prevent fractures occurring in the first place, than to treat the consequences of fractures, which are not only physical but also psychological traumatic.
Menopause can occur at any age, the average is 51, but it can occur in the 20 and 30’s. The most common cause of bone loss in women is low levels of the sex hormone oestrogen, which keeps bones healthy and strong, and it naturally declines during menopause. If women are also under a lot of stress, which dealing with the menopause itself is very stressful, this will also lower their oestrogen levels. As a result, they lose even more bone and the majority of people who contact the IOS have a minimum of 3 risk factors contributing to their bone loss.
Osteoporosis is unlike many diseases, in that it is linked to so many other conditions or diseases, treatments and medications, as well as poor lifestyle choices, which is one of the reasons why many who contact the IOS have 3 to 6 risk factors for bone loss.
Why prevention of bone loss is essential
Osteoporosis medications can help to reduce fracture risk by up to 70%.
Osteoporosis medications can help to reduce fracture risk by up to 70%.
Ireland has the 6th highest hip fracture rate in the world.
A women’s risk of fracture is greater than her combined risk of cardiovascular disease and breast cancer.
More women die from the complications of osteoporosis fractures than the combined deaths from cancer of the ovaries, uterus and cervix.
Approximately 48,000 fractures occur in Ireland annually. In 2022, 72,852 acute hospital bed days were occupied by hip fracture patients. That same year the cost of one hip fracture was ¤12,425 with 3,909 hip fractures occurring at a cost of ¤45,569,325. 69% were women, 84% were admitted from their homes, with 49% having a high function ability mobility score prior to fracturing.
20% of people aged 60+ who fracture their hip will die within six -12 months, 50% will lose the ability to wash and dress themselves, and to walk across a room unaided.
It is the secondary consequences of a fracture that can cause death, such as pneumonia, blood clot, or infection.
The life expectancy in 1995 was 75 years and by 2030 the estimated life expectancy is 84. We already have a bone health crisis and with our population ageing there is going to be a bone health tsunami, therefore preventing those at risk not only makes ethical sense but also monetary.
Many vertebral fractures are not diagnosed and are asymptomatic, with only one third of all vertebral fractures clinically diagnosed. There is an increased mortality and morbidity rate similar to hip fractures, however obvious associations with specific causes of death have so far not been reported. Increased mortality has also been found in some studies to be independently associated with low bone mineral density without fractures.
A lateral thoracic Xray is the first line for diagnosing vertebral fractures, however, a DXA is necessary to monitor the bone loss and the patient’s response to treatment.
FRAX: There are approximately 200 causes of bone loss, and unfortunately FRAX only lists 12. Vitamin D deficiency, increased bone turnover, frailty and falls are not included on it. For those who do not deal with many Osteoporosis patients, it is a helpful tool. A detailed questionnaire is more through and will pick up on additional risk factors, which is available from the IOS info@irishosteoporosis.ie
The images below show the horrific, irreversible skeletal damage that occur at any age due to vertebral fractures.
What osteoporosis treatment a person is put on should depend on
• Clinical judgement of the treating physician
• The causes of their bone loss which should be investigated and addressed, not assumed. Examples menopause or steroids.
• If they have fractured already
• Their DXA scan results of their spine and hips
• The patient’s ability to swallow tablets or ability to self-inject
• Contraindications to any of the treatments
• The patient’s cognitive ability
• Results from blood tests, Vitamin D being one of the most crucial
• Their medical history
• Their age

Osteoporosis medications should always be used in combination with:
• Calcium and vitamin D, preferably through food
• A well-balanced diet with adequate calories including first class proteins
• Adequate Fluid (preferably water) intake at least one and half to 2 litres a day
• Stopping smoking
• Reducing excessive caffeine, alcohol and fibre intake
• 30 minutes of safe and appropriate weight bearing exercise daily for adults, 60 minutes for children, suitable for their age, ability and DXA results.
• Reducing stress levels
NOTE: The concept of yoga is wonderful, but it was developed without the knowledge we now have and the IOS do not recommend it for anyone with and without bone loss.
NOTE: Reducing stress is essential, as stress can affect sex hormone levels which will cause bone loss.
Patients who have not sustained a fracture
• Investigate and address cause/s of bone loss
• Prevent further bone loss and reduce the risk of fracture by putting a bone health plan in action
• Treating those who are high risk preventatively
• Refer to chartered physiotherapist for a safe and appropriate weight bearing and core strengthening exercise programme
Patients who have sustained a fracture
• Investigate and address cause/s of bone loss
• Prevent further bone loss
• Reduce the risk of further fractures
Reduce pain and disability associated with fractures
Reduce risk of losing independence
Reduce risk of premature death
• Refer to chartered physiotherapist for a safe and appropriate weight bearing and core strengthening exercise programme
NOTE: A person may have a T score of -1.8 but if they have had a major fragility fracture, they should be considered to have Osteoporosis, unless proven otherwise and prevention of further fractures is crucial.
Treatments
There are two main types of medications, antiresorptive and anabolic.
Antiresorptive medications
These slow down the formation of osteoclasts, the cells that break down bone, these include the Bisphosphonates, Denosumab, SERMS (selective oestrogen receptor modulators) and to a lesser extent HRT.
Anabolic medication
These stimulate the osteoblasts cells that build up new bone. Treating patients with fractures or very low bone density with anabolic medication and antiresorptive drugs will achieve higher bone mineral density earlier, which reduces their risk of further fractures very quickly.
Bisphosphonates
There are several forms of Antiresorptive medications
1) Weekly tablets
2) Monthly tablets
3) By IV once a year
Bloods measuring PTH, vitamin D, calcium, renal function and ideally bone turnover markers should be done. Ideally the vitamin D levels should be 70 up to 125nmol/L, with a normal level of PTH, as high PTH levels cause bone loss.
Bisphosphonates are nonhormonal drugs that have to be incorporated into bone and can help to reduce the risk of fractures in the spine and hips in postmenopausal women and men.
Bisphosphonates have their place in treating patients but unfortunately, they are poorly absorbed, and they form mosaic bone, not normal bone. It is essential that they are taken with the person upright or standing/ walking. One of the issues is that over the last several years the amount of people contacting the
IOS saying they are unable to tolerate them has drastically risen to approximately 70%, which significantly affects compliance. Approximately 20% are put on protein pump inhibitors to counteract the stomach issues they developed taking them, which is counterproductive because they cause bone loss.
Oral bisphosphonates should not be given to patients who have any of the following
Absorption issues, Hiatus hernia, Oesophageal abnormalities such as reflux, Barrett’s Oesophagus, impaired renal function or ulcers.
NOTE: Currently it is recommended that you do not take bisphosphonates for more than a total of 5 years, not 5 years on each one. Consideration should be taken for those who may be able to d/c Prolia by keeping 1 of these 5 years to close off the action of Prolia.
Denosumab (Prolia) is an antiresorptive medication. It is a Monoclonal antibody which binds to RANK Ligand inhibiting the maturation of osteoclasts, thus protecting the bone from degradation, preventing bone loss and osteoporosis. It does not have to be incorporated into bone, which is why It forms normal bone.
Prolia reduces the risk of vertebral, non-vertebral and hip fractures.
It is given as a Subcutaneous injection 60mg, given 6-monthly. It is approved for postmenopausal women at high risk to fracture and men and women who are undergoing chemotherapy, radiation and sex hormone ablation therapy, to prevent bone loss.
Bloods measuring PTH, vitamin D, calcium, renal function and ideally bone turnover markers should be done before each injection. Ideally the vitamin D levels should be 70 up to 125nmol/L, with a normal level of PTH.
NOTE: It is essential that the patient drinks adequate fluids to prevent urinary tract infections.
Prof O’Brien stated “Hypocalcaemia is a contraindication and Prolia is suspended in a lactose solution. Patients who were very allergic to lactose may have a reaction to Prolia. I have only had a couple of patients who are extremely sensitive to lactose that were not able to tolerate it”.
Patients on Prolia should take it preferably six months to the day of their last injection. The maximum delay after the due date for the injection should be four weeks to prevent the rebound increase in bone loss, which can result in spontaneous vertebral fractures. Pharmacists can assist by noting the dates the injection was picked up.
NOTE: An antiresorptive medication e.g. an IV bisphosphonate must be prescribed if Prolia is being discontinued to close off the action of Prolia on bone, to prevent an increase in bone loss, which would result in vertebral fractures. The marked increase in Bone marker CTX1 will reflect this risk. No patient should ever be put on a Prolia drug holiday.
Teriparatide (Parathyroid hormone) is an anabolic bone forming agent, that stimulates the formation of new bone. It can only be prescribed by a consultant, as it is a High-Tech drug for severe osteoporosis. It is given as a daily 20mcg, subcutaneous injection in the thigh or abdomen for 12/24 months. Teriparatide is usually recommended for those with spinal fractures and/or very low bone density. It also helps to prevent bone loss for people on corticosteroids and reduces vertebral and nonvertebral fractures in women.
Prof O’Brien stated “Teriparatide was not developed to decrease pain but 95% of my patients experience a significant decline in vertebral fracture pain after several weeks on the treatment. Many of these patients would have been put on morphine patches prior to seeing me, which 85% would have reported no decline in their fracture pain level from morphine”.
It is contraindicated in patients who have had radiation, have multiple myeloma, Paget’s disease, are pregnant or breast feeding. It is essential that the patient has normal vitamin D, Parathyroid hormone levels, normal calcium, liver and kidney function.
HRT – Hormone replacement therapy or the contraceptive pill
Oestrogen/progesterone hormone therapy Sex hormones play a vital role in determining the onset of osteoporosis. Both testosterone in males and female hormone oestrogen have a protective effect on bones and help prevent the breakdown of bone.
The normal age of menopause (no periods for one year) is usually in the early 50s, if it occurs below 45 years it is considered an early menopause.
Menopause is a major cause of osteoporosis due to oestrogen deficiency, which causes many women to develop symptoms such as hot flushes, difficulty with sleep, vaginal dryness, sweats, mood changes and brain fog. This usually increases stress levels (cortisol levels), which causes further bone loss.
HRT is usually recommended for postmenopausal symptoms to help improve the person’s quality of life and their families! Patients should be informed of the benefits and negative effects of HRT treatment, and they should be monitored.
HRT is usually the first choice for treatment of menopausal symptoms provided there are no contraindications. It is usually not recommended just for the prevention and treatment of osteoporosis, unless the person has an early menopause.
HRT is not suitable for people who have a family history of breast cancer, particularly if there is a history of deep vein thrombosis.
Prof O’Brien stated “Teenagers with eating disorders may not have started having periods or will have lost their periods and have very low oestrogen and progesterone levels. Those I have treated with severe bone loss have Z scores of -3.5 to -5.5, on a DXA machine using special paediatric software. Example: I have 18 year olds with vertebral fractures. For optimal results, any male or female with an eating disorder should be referred for a DXA scan urgently.
HRT Oestrogen on its own is available in many forms including tablets, skin patches and gels but is usually combined with a progestogen, a synthetic version of the hormone progesterone and this may be in the form of a coil. Oestrogen on its own should only be used by women who have had a hysterectomy.
It may be used as a sequential combined therapy; oestrogen is taken every day and progestogen for approximately 12 days which should result in menstrual bleeding. Continuous combined therapy is when both oestrogen and progestogen are taken every day as a result there are no periods, this should not be started until they have had no periods for a year.
Selective Oestrogen Receptor Modulators (SERMS)
SERMS: Tamoxifen, Raloxifene, they are not oestrogen but have some similar to oestrogen increasing oestrogen levels in bone and preventing osteoporosis mainly in the spine.
Tamoxifen is also used in the treatment of ER positive breast cancers.
Raloxifene is usually prescribed for postmenopausal women provided they have no contraindications, particularly a history of deep vein thrombosis and pulmonary loss.
It is 60 mg tablet taken once a day.
NOTE: It should not be given to women who are experiencing hot flushes as it will increase them or to pregnant women.
Romosozumab (EVINITY)
NOTE: It is a High-Tech drug which is available in the US and Europe and hopefully will be available soon in the Republic of Ireland.
It is another type of antiresorptive drug which is a monoclonal antibody against Sclerostin, this is the first anabolic medication that increases bone formation and decreases bone resorption.
It is licensed for postmenopausal women who have had osteoporotic fractures or are at high risk of fractures. it is a monthly subcutaneous injection that is given in 2 separate injections for one year. Contraindications in those with hypocalcaemia, a history of stroke or myocardial infarction or sensitivity to the substance.
Summary
All patients need to be monitored as bone loss is silent and currently DXA scanning is the most efficient way.
Osteoporosis is treatable and fractures are preventable, but one low trauma fracture increases the risk significantly of a second fracture in the next year if not diagnosed and treated.
Postmenopausal white women are the highest risk group affected, but it can occur at any age in both males and females, and all races. Effective treatments have been available for more than a decade; however, research shows that most people who fracture, or are at risk of fracture, are never assessed or treated for their underlying osteoporosis, and they go on to have additional fractures and the associated morbidity.
All medications have possible side effects but the benefits to bone health by preventing future fractures, skeletal deformities, loss of independence and possibly premature death, usually far outweigh the risk of a side effect.
Please make bone health a major priority in Ireland and help the IOS to ensure that people age with their dignity intact and fracture free, in order that they can actually enjoy their retirement.
Written by Michele O’Brien, CEO of the Irish Osteoporosis Society and Professor Moira O’Brien, Osteoporosis Consultant, Affidea Dundrum, DublinWritten by Michele O’Brien, CEO of the Irish Osteoporosis Society and Professor Moira O’Brien, Osteoporosis Consultant, Affidea Dundrum, Dublin
Read our latest Features









